Robles Lab Shedding New Light
Sep 24, 2018 — Atlanta, GA
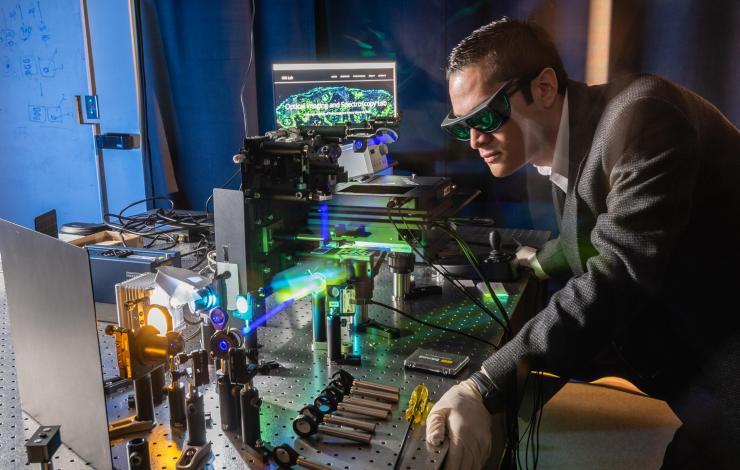
Francisco Robles
Francisco Robles’ research sheds light and brings clarity to a microscopic world, and two recently published papers continue his lab’s ambitious goals to advance optical technologies that improve our understanding of biological processes.
But while both projects share a common umbrella, they are independent of each other and fulfill completely different needs.
With “Ultraviolet Hyperspectral Interferometric Microscopy” in the Nature journal, Scientific Reports, Robles and his collaborators introduce ultraviolet hyperspectral interferometric (UHI) microscopy, an affordable system for molecular imaging that overcomes the challenges typically associated with UV spectroscopy.
In “Dual-wavelength oblique back-illumination microscopy for the non-invasive imaging and quantification of blood in collection and storage bags,” in Biomedical Optics Express, the research team developed a system to quantitatively assess the suitability of cord blood for stem cell therapy applications, while saving time and dramatically cutting costs for blood banking.
UHI is a novel tool developed by Robles, assistant professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University, and a researcher in the Petit Institute for Bioengineering and Bioscience at Tech. It’s a microscopy technique that probes unique endogenous absorptive and scattering properties of cells and tissues in the deep ultraviolet (deep-UV) region of the spectrum.
“The use of deep-UV light for microscopy offers many potential advantages over traditional methods,” the research team noted in Scientific Reports. “Unfortunately, there have been a number of challenges that have hampered progress in this area, including less than optimal cameras and light sources, phototoxicity, strong fluorescent background, and severe chromatic aberration.”
But as the team points out in the paper, UHI microscopy leverages recent advances in technology and research to overcome these challenges.
“We have developed a versatile instrument that, to our knowledge, is the first to achieve hyperspectral imaging in the deep-UV, with access to attenuation and dispersion properties, and quantitative phase,” the researchers wrote. “The capabilities afforded by UHI microscopy overcome significant limitations that have plagued deep-UV microscopy, and offer new opportunities for highly-sensitive, label-free imaging.”
Typically, label-free molecular imaging has been accomplished through fluorescence microscopy or non-linear microscopy, which have a limited number of molecular targets or requiring expensive systems. Robles expects the information provided by the more cost-effective UHI microscopy to yield unprecedented insight into a wide range of molecules and phenotypes. “We’re talking about fewer dollar signs,” he said. “And the approach can potentially be used to improve prognosis of all cancers.”
The work was supported largely by a 2017 National Science Foundation (NSF) CAREER Award, for early career faculty researchers, won by Robles, principal investigator of the Optical Imaging and Spectroscopy (OIS) Lab at Georgia Tech and Emory.
In addition to Robles, other authors of the paper were Wilbur Lam (associate professor in the Coulter Department and a Petit Institute researcher); Ashkan Ojaghi (lead author and a graduate student in the Robles lab); and Meredith Fay (graduate student in Lam’s lab).
Saving Blood and Money
The research outlined in Biomedical Optics Express (the journal of the Optics Society) addresses a different kind of expensive process. Traditionally, there hasn’t been a low-cost method to quantitatively assess the contents of a blood bag without breaching the bag and potentially damaging the sample. So the Robles team adapted a technique called oblique back-illumination microscopy (OBM) to rapidly, inexpensively, and non-invasively screen blood bags for red blood cell morphology and white blood cell count.
“The goal here is to get really high contrast of cells, which are actually transparent, so that we can identify certain types of cells in blood,” said Robles. “What we’re really after are mononuclear cells in umbilical cord blood.”
Mononuclear cells (MNCs) are important components of the body’s immune system, and often used in research and clinical applications (including microbiology, virology, oncology, vaccine development, transplant and regenerative biology, and toxicology). For this paper, the Robles lab collaborated with Joanne Kurtzberg, a renowned researcher at Duke University, where she runs the Carolinas Cord Bank, one of the largest public cord banks in the world.
When cord bankers collect blood from a donor (a non-invasive, no-risk procedure), they want to isolate these valuable MNCs, but it hasn’t been an efficient process, and about 75 percent of the blood bags wind up being discarded.
“Cord blood banking is about 10 times more expensive than other sources of blood for stem cell therapy, and that should not be the case,” said Robles.
His team employed OBM, a recently developed imaging technique that provides tomographic differential phase contrast, to image and quantify the contents of a blood bag, “a simple, low-cost operation, without touching the blood or rupturing the bag, without wasting any blood whatsoever,” Robles said.
It takes about a minute to get an accurate estimate of the useful cells in a batch of blood right there in the hospital when it is collected.
Co-authors of the paper, in addition to Robles and Kurtzberg, were lead author Patrick Ledwig (a graduate student in the Robles lab) and Moses Sghayyer (a former undergraduate researcher in the Robles lab). The research was supported by, among others, the North Carolina-based Burroughs Wellcome Fund and the Marcus Center for Therapeutic Cell Characterization (MC3M) at Georgia Tech.
“Our images have been so fantastic that we’re expanding the technology to look at other types of environments,” Robles said.
For example, another use of the technology could determine the viability of blood stored for transfusions. This blood is usually stored for 42 days, then thrown away, “an arbitrary cutoff,” Robles said.
“It may be that the blood is no longer useful, and it may be useful beyond that point. We can quickly diagnose it with this system,” Robles said. “And we can start studying diseases like sickle cell disease and leukemia. There are many different avenues. We can look at thousands and thousands of cells very quickly to get a better understanding of disease.”
Jerry Grillo
Communications Officer II
Parker H. Petit Institute for
Bioengineering and Bioscience




