Flicker Treatment for Alzheimer’s Gets a Test Run
Nov 13, 2020 — Atlanta, GA
Researchers at the Georgia Institute of Technology and Emory University have reported promising results from a small initial human feasibility trial studying the effects of flickering light and pulses of sound in the treatment of Alzheimer’s disease. Annabelle Singer, the principal investigator from Georgia Tech, presented the work on Friday, Oct. 9, at the American Neurological Association annual meeting.
“This stimulation harnesses our brain’s natural tendency to entrain to stimuli, to then manipulate neural activity, recruit the brain’s immune system, and clear pathogens,” Singer explained to a virtual audience in her recorded video presentation.
The work is based on previous animal studies by Singer and her colleagues, in which they discovered that a light flickering at 40 hertz (40 cycles per second) stimulates gamma waves, significantly cutting down on amyloid beta, an Alzheimer’s pathogenic hallmark. Gamma waves are associated with high-level cognitive functions, like perception and memory. Disruptions to these kinds of brain waves have been found in various neurological disorders.
“We found that one hour of gamma stimulation reduced amyloid beta and recruited microglia, the primary immune cells of the animals’ brains,” said Singer, assistant professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory. She added that the treatment, “even rescued spatial memory behavior in mice. That led to our next key question. Does this translate to humans?”
To answer that question, Singer initiated the Phase I feasibility trial with James Lah, principal investigator of the study for Emory, where he is associate professor and vice chair in the Department of Neurology and director of the Cognitive Neurology Program.
“We went into this preliminary pilot study with the primary goal of learning whether or not sustained use of this device would be tolerable in humans, and whether or not people would use it,” Lah explained. “The results were promising. Everybody tolerated the devie and we were able to tune it to the level of light and sound that was not only tolerable, but successfully provoked the underlying brain response that was desired.”
The initial feasibility study, an eight-week trial entitled, “Gamma Sensory Flicker for Patients with Prodromal Alzheimer’s Disease: A Phase I Trial,” involved 10 people who were organized into two groups of five each. One group underwent no flicker treatments for the first four weeks, followed by four weeks of treatment. The other group received eight weeks of flicker treatments.
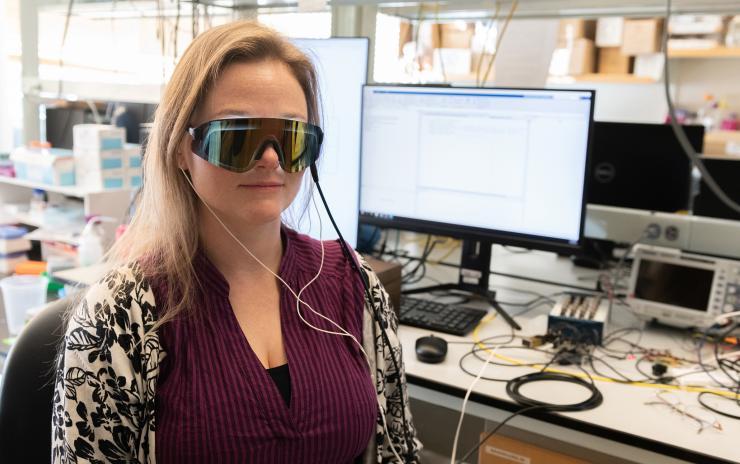
First, the research team assessed the safety of treatment, which required participants to wear an experimental visor and head phones that exposed them to 40 Hz of light and sound. There were no overall severe adverse events among participants during pre-trial screening, in the study, or during the 10-month open label extension (some patients volunteered to continue being monitored and assessed). There were some mild adverse effects that could be flicker related (dizziness, tinnitus, headache, worsened hearing loss). But overall, Singer said, the safety profile was excellent.
Of major concern to the researchers was whether participants would tolerate the treatment, and stick with it over eight weeks or more. Again, Singer and her team were satisfied with the results: Most participants tolerated it well, and adherence was greater than 88 percent among all participants.
The researchers found that there were no clear changes in the presence of Alzheimer’s pathogens (amyloid beta and p-Tau), but saw strong EEG entrainment (brain wave synchronization) at 40 Hz when gauging participants’ neural responses during flicker, and a significant increase in neural network functional connectivity (which is weakened in Alzheimer’s) after eight weeks.
Also, as they had previously observed in studies with mice, the researchers noted the activity of cytokines (small proteins used in cell signaling), which indicated that flicker is also engaging the brain’s immune system in humans.
“These are interesting but preliminary biological effects of gamma flicker,” Singer said. “All of this is gearing us up for our next larger and longer study coming soon.”
The study was funded by the National Institute of Neurological Disorders and Stroke at the National Institutes of Health (R01-NS109226-01S1), by the Packard Foundation, the Friends and Alumni of Georgia Tech, the Lane Family, the Wright Family, and Cognito Therapeutics. Any findings, conclusions, and recommendations are those of the researchers and not necessarily of the sponsors.
Competing interests: Annabelle Singer owns shares in Cognito Therapeutics, which funded the human study at Emory Brain Health Center. Cognito aims to develop gamma stimulation-related products. These conflicts are managed by Georgia Tech’s Office of Research Integrity Assurance.




